How AI Helps Reduce Patient Attrition in Healthcare Systems
Advanced Predictive Analytics in Medicine
Modern machine learning systems demonstrate exceptional proficiency in processing complex medical datasets, uncovering subtle correlations that often escape human observation. This analytical capability enables anticipating health trends and potential outcomes across multiple clinical scenarios. The true value of these systems lies in their capacity to derive insights from past patient interactions and apply them to forecast future healthcare needs. Such foresight empowers medical teams to implement preventive strategies and optimize treatment protocols.
Proactive Healthcare Strategies
Within clinical settings, predictive analytics tools play a crucial role in identifying patients vulnerable to specific health conditions. Through comprehensive evaluation of medical histories, behavioral patterns, and genetic markers, these systems can pinpoint individuals requiring early intervention. Timely medical attention based on predictive analysis not only enhances treatment efficacy but also generates substantial savings for healthcare institutions. This preventive model represents a paradigm shift from reactive to proactive medicine.
Enhancing Financial Security
Advanced analytical systems demonstrate remarkable proficiency in detecting irregular patterns within healthcare billing systems. By monitoring treatment patterns, service utilization, and payment behaviors, these tools can flag potentially fraudulent activities. Such vigilance is essential for maintaining the financial health of medical institutions while protecting patients from improper billing practices. The implementation of these systems has become an industry standard for risk mitigation.
Supply Chain Optimization
Predictive analytics significantly improves medical supply management by forecasting potential shortages and optimizing inventory distribution. Analyzing variables including seasonal disease patterns, regional health trends, and equipment utilization rates enables more accurate demand prediction. This forward-looking approach allows healthcare facilities to prevent critical supply shortages while minimizing wasteful overstocking. The resulting efficiency gains translate to better patient care and reduced operational costs.
Resource Utilization Strategies
Intelligent systems provide healthcare administrators with powerful tools for maximizing resource efficiency. From energy management in medical facilities to staff scheduling optimization, these solutions analyze operational data to identify improvement opportunities. Data-driven resource allocation leads to measurable cost reductions while promoting environmentally sustainable healthcare delivery. These efficiency gains directly benefit both institutions and patients.
Patient Support Systems
AI-enhanced communication tools have revolutionized patient interactions by providing immediate responses to common inquiries. Through continuous analysis of patient feedback and service interactions, these systems continually refine their support capabilities. Personalized digital assistance significantly improves patient satisfaction while reducing administrative burdens on medical staff. This dual benefit makes such implementations increasingly valuable in modern healthcare.
Safety Enhancement Technologies
Modern analytical systems contribute substantially to improving safety protocols in medical environments. Through pattern recognition and anomaly detection, these tools help prevent adverse events before they occur. Proactive safety monitoring protects both patients and healthcare professionals while reducing institutional liability. From medication error prevention to facility security, these applications are transforming safety standards in healthcare.
Customizing Healthcare Interactions Through Personalization
Comprehensive Patient Assessment
Contemporary healthcare delivery requires understanding each patient's unique circumstances beyond their immediate medical needs. Effective care considers psychological, socioeconomic, and cultural factors that influence health behaviors and treatment adherence. These contextual elements often determine the success of medical interventions as much as the clinical protocols themselves.
Truly personalized care involves active listening that extends beyond verbal communication. Care providers must develop sensitivity to subtle cues in body language, emotional tone, and personal circumstances. This holistic understanding enables medical professionals to tailor their approach to each individual's specific situation and expectations.
Adaptive Communication Approaches
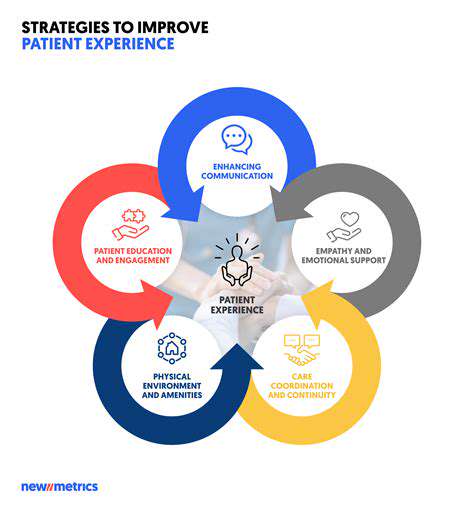
Building patient trust requires clear, jargon-free explanations of medical conditions and treatment options. Effective healthcare communication balances technical accuracy with accessibility, ensuring patients can make fully informed decisions about their care. Encouraging questions and confirming understanding should be standard practice in all clinical interactions.
Therapeutic Environment Design
The physical and emotional atmosphere of healthcare facilities significantly impacts patient experiences. Thoughtful environmental design can dramatically reduce stress levels and improve clinical outcomes. Considerations ranging from color schemes and lighting to privacy measures and comfortable furnishings all contribute to creating healing environments.
Involving support networks in care processes often enhances treatment effectiveness, particularly for patients facing complex medical challenges or cognitive difficulties. Family participation can improve medication adherence and follow-through with treatment recommendations.
Operational Efficiency Improvements
Bureaucratic hurdles represent a major source of patient dissatisfaction in healthcare systems. Implementing digital solutions for appointment management, records access, and billing inquiries can dramatically improve the patient experience while reducing administrative costs.
Digital Health Integration
Modern patients increasingly expect healthcare services to match the convenience of other digital experiences. Patient portals for scheduling, prescription management, and provider communication have become essential components of contemporary medical practice. Telehealth options extend access to care while reducing burdens on both patients and healthcare facilities.
Strategic Resource Management in Healthcare
Personalized Patient Engagement Strategies
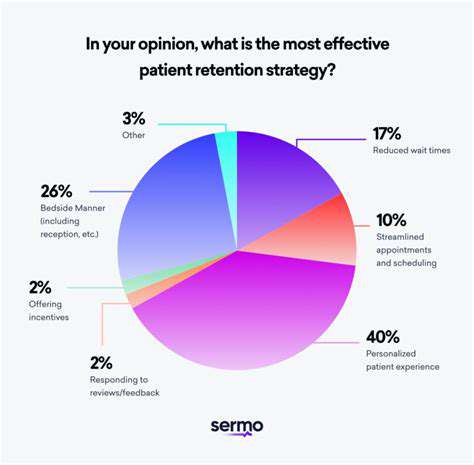
Advanced analytics systems can evaluate individual patient characteristics to customize communication approaches. Tailored appointment reminders, condition-specific educational materials, and personalized follow-up protocols demonstrate the healthcare system's commitment to individual needs. By addressing patient preferences through customized interactions, providers can significantly improve treatment adherence and health outcomes while reducing costs associated with patient attrition.
This individualized approach minimizes unnecessary clinical interactions while maximizing the impact of essential interventions. Proactive identification and resolution of potential issues fosters stronger patient-provider relationships and reduces the likelihood of patients seeking alternative care options.
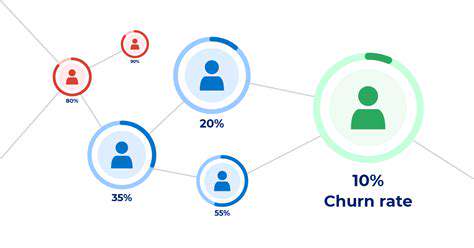
Early Identification of Vulnerable Patients
Predictive analytics can process comprehensive patient profiles to identify those at elevated risk of discontinuing care. This capability enables timely, targeted interventions that address potential barriers to continued treatment, potentially preventing costly patient loss and ensuring continuity of care.
Early detection of at-risk patients allows for implementation of customized support measures, ranging from modified communication strategies to adjusted care plans. This preventive model represents a cost-effective approach to patient retention by focusing resources where they're most needed.
Administrative Process Optimization
Automation of routine administrative tasks through intelligent systems allows healthcare staff to dedicate more time to direct patient care. The resulting efficiency gains translate to both improved clinical outcomes and substantial operational cost reductions through decreased administrative overhead.
Streamlined administrative workflows reduce processing errors and delays, enhancing both financial performance and patient satisfaction. These operational improvements create resources that can be reinvested in quality improvement initiatives.
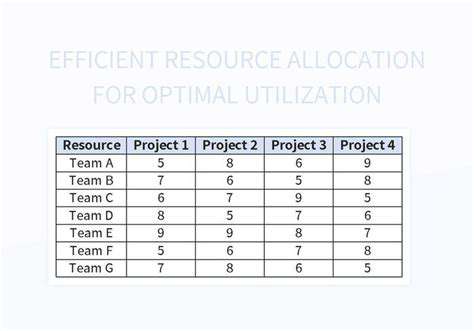
Precision Resource Allocation
Data-driven analysis enables healthcare administrators to identify the most effective distribution of limited resources. By recognizing patterns in treatment responses and patient behaviors, institutions can focus interventions where they'll produce the greatest impact on patient retention and health outcomes.
This evidence-based approach to resource management ensures optimal utilization of healthcare budgets while maintaining high standards of patient care. The resulting efficiency gains support sustainable healthcare delivery models in an era of increasing cost pressures.