Understanding Predictive Modeling in Healthcare
Modern predictive analytics transforms raw patient data into actionable clinical insights. By examining patterns across thousands of variables—from lab results to social determinants—these systems can forecast health trajectories with remarkable accuracy. This capability enables providers to shift from reactive to proactive care models, intercepting potential complications before they escalate.
The true power lies in identifying subtle correlations human analysts might overlook. For instance, an algorithm might detect that patients with specific medication adherence patterns combined with certain vital sign fluctuations face elevated readmission risks, prompting targeted interventions for those individuals.
The Role of AI in Enhancing Predictive Accuracy
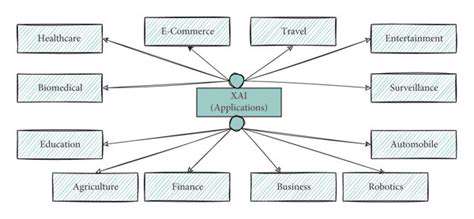
Artificial intelligence acts as a force multiplier for healthcare analytics, processing complex datasets at scales impossible for human teams. Machine learning algorithms continuously refine their predictive models as they ingest new data, becoming increasingly precise over time. This dynamic improvement cycle helps healthcare systems stay ahead of emerging health trends and evolving patient needs.
AI's pattern recognition capabilities prove particularly valuable for synthesizing information from disparate sources—electronic records, wearable devices, even unstructured physician notes. By finding connections across these data streams, AI models provide clinicians with comprehensive risk assessments that inform personalized care strategies.
Identifying High-Risk Patients: A Practical Application
Consider postoperative care as a prime use case. Predictive models can analyze hundreds of preoperative and intraoperative factors to forecast recovery complications. This enables surgical teams to tailor discharge plans and follow-up protocols based on each patient's predicted risk profile, potentially preventing emergency readmissions.
Chronic disease management represents another critical application area. By identifying patients trending toward diabetes or cardiovascular events months before traditional diagnostic criteria would flag them, providers can implement lifestyle interventions that may prevent disease onset entirely.
Ethical Considerations and Data Privacy
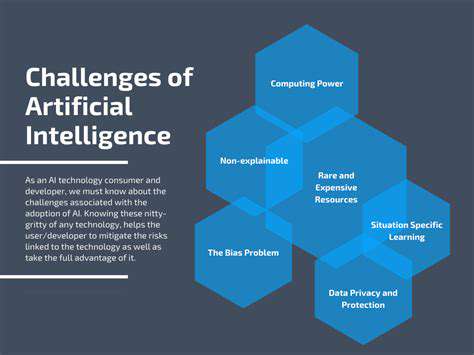
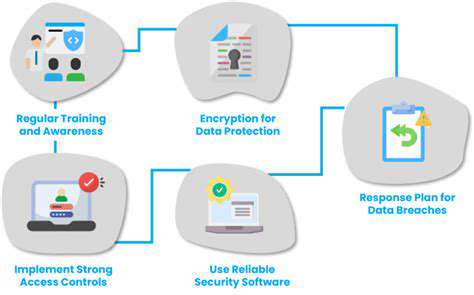
While predictive analytics offers tremendous potential, it introduces complex ethical dilemmas that demand careful navigation. Algorithmic bias represents a particularly insidious risk, as models trained on non-representative data may perpetuate healthcare disparities. Rigorous auditing processes must ensure predictions remain equitable across demographic groups.
Transparency presents another crucial consideration. Clinicians need to understand how models generate predictions to appropriately weigh their recommendations. Developing explainable AI systems that balance predictive power with interpretability remains an ongoing challenge for the field.
Personalized Discharge Planning and Post-Discharge Support

Personalized Discharge Planning: A Holistic Approach
Truly effective discharge planning recognizes that medical needs represent just one facet of recovery. A comprehensive approach considers patients' living situations, support networks, financial constraints, and health literacy levels. This multidimensional assessment ensures transition plans align with each individual's reality rather than idealized scenarios.
Active patient and family engagement transforms discharge from a bureaucratic process into a collaborative care strategy. When patients help design their post-hospitalization plans, they demonstrate better understanding and adherence—critical factors in preventing readmissions.
Developing a Patient-Centered Plan
Crafting an effective discharge strategy requires digging beyond surface-level assessments. Clinicians must understand whether patients can afford prescribed medications, have transportation to follow-up appointments, or possess the physical capability to complete recommended therapies. These practical considerations often prove more consequential than clinical factors in determining recovery success.
The planning process should incorporate patient preferences and values whenever possible. Some individuals may prioritize returning to work quickly, while others focus on pain management or regaining specific functional abilities. Aligning the discharge plan with these personal goals improves engagement and outcomes.
Incorporating Technology and Resources
Digital tools are revolutionizing post-discharge support. Remote monitoring platforms allow clinicians to track recovery progress between visits, while medication adherence apps help patients stay on schedule with complex regimens. These technologies create virtual safety nets that prevent minor issues from becoming readmission-worthy crises.
Community partnerships extend care beyond clinical settings, connecting patients with local services that address social determinants of health. From meal delivery programs to transportation services, these resources help overcome non-medical barriers to successful recovery.
Addressing Potential Barriers to Discharge
Proactive problem-solving distinguishes exceptional discharge planning. Identifying potential obstacles—like limited health literacy or unstable housing—allows care teams to implement solutions before they derail recovery. This might involve arranging temporary housing, providing illustrated medication instructions, or scheduling transportation assistance.
Early intervention for high-risk patients can dramatically reduce readmission rates. Flagging social or environmental risk factors during hospitalization enables care teams to mobilize appropriate support systems before discharge occurs.
Evaluating and Modifying the Plan
Discharge planning represents an ongoing process rather than a one-time event. Regular check-ins allow for plan adjustments as patients' needs evolve during recovery. This adaptive approach ensures support remains relevant through each phase of the healing process.
Patient feedback provides invaluable insights for improving discharge processes. Systematic collection of patient experiences—both positive and negative—helps institutions refine their approaches to better serve future populations.
Ensuring Continuity of Care
Seamless care transitions require meticulous information sharing between hospital teams and community providers. Standardized handoff protocols prevent critical details from falling through cracks during care transitions. Electronic health record systems play a vital role in maintaining this continuity, though human verification remains essential.
Clear communication channels between acute and outpatient providers create safety nets for recovering patients. When primary care physicians receive comprehensive discharge summaries and know how to contact hospital teams with questions, they can provide more confident, coordinated follow-up care.
Optimizing Resource Allocation and Care Coordination
Improving Patient Flow
Advanced analytics transform patient flow management from reactive to predictive. By modeling historical patterns and real-time data, hospitals can anticipate surges and adjust operations accordingly. This might involve opening additional units during predicted peak periods or strategically staggering elective procedures to smooth demand curves.
These data-driven approaches yield substantial efficiency gains, reducing both patient wait times and staff frustration. Optimized flow management also decreases costly overtime expenditures while improving care quality through more consistent staffing ratios.
Enhancing Care Coordination
Predictive analytics bridges traditional silos between specialties and care settings. Shared data platforms give all providers—from emergency physicians to home health nurses—a unified view of each patient's status and needs. This transparency prevents redundant testing and ensures all team members work toward aligned goals.
The resulting care continuity particularly benefits patients with complex, chronic conditions who might otherwise receive fragmented care across multiple disconnected providers.
Optimizing Staffing Levels
Sophisticated workforce forecasting tools analyze countless variables—from seasonal illness patterns to local event calendars—to predict staffing needs with remarkable precision. This allows nurse managers to adjust schedules proactively rather than scrambling to cover unexpected absences or surges.
Strategic staff allocation also improves job satisfaction by reducing burnout from chronic understaffing while avoiding the financial and morale costs of excessive overtime.
Reducing Hospital Readmissions
Predictive models identify not just who might need readmission, but why. This insight allows for targeted interventions—whether additional education for patients prone to medication errors or enhanced social work support for those with unstable home environments. Addressing root causes proves far more effective than generic prevention strategies.
The financial implications are substantial, as preventable readmissions represent one of healthcare's most significant cost drivers. Effective prediction and prevention strategies can yield savings that fund other quality improvement initiatives.
Improving Resource Allocation
From imaging equipment to specialty beds, predictive analytics ensures critical resources are available when and where needed most. Real-time tracking combined with usage pattern analysis allows for dynamic reallocation as needs shift throughout each day.
This precision resource management reduces both equipment underutilization and patient delays, creating leaner operations that deliver better care at lower costs.
Predicting Demand and Capacity
Long-term predictive modeling helps hospital administrators make informed strategic decisions about facility expansions, service line investments, and partnership opportunities. By anticipating community health needs years in advance, institutions can evolve their service offerings proactively rather than reactively.
This forward-looking approach creates healthcare systems that grow sustainably while remaining responsive to their populations' changing needs.
The Future of Hospital Readmissions: A Data-Driven Approach
Reducing Readmission Rates Through Proactive Care
The readmission crisis demands fundamentally rethinking how we approach care transitions. Proactive strategies that begin at admission and extend well beyond discharge offer the most promising path forward. This includes embedding prevention specialists in care teams and redesigning workflows to prioritize continuity.
Empowered patients become active partners in preventing readmissions. When individuals understand their conditions and feel confident managing them, they're far less likely to require emergency returns to the hospital.
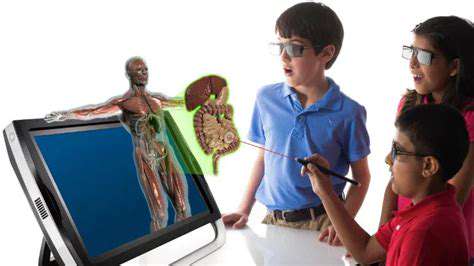
Technological Advancements in Patient Monitoring
Next-generation remote monitoring moves beyond simple vital sign tracking to comprehensive health ecosystem analysis. Smart homes equipped with non-invasive sensors can detect subtle changes in activity patterns, sleep quality, and medication adherence that signal emerging problems.
These ambient monitoring technologies provide continuous health surveillance without burdening patients with wearable devices or frequent self-reporting, creating seamless safety nets for vulnerable populations.
Improving Post-Discharge Follow-up
Automated follow-up systems ensure no patient falls through the cracks after discharge. Intelligent scheduling algorithms determine optimal check-in timing based on individual risk factors, while natural language processing analyzes patient responses for concerning patterns that might warrant intervention.
This combination of automation and clinical oversight creates scalable systems that provide personalized attention to thousands of recovering patients simultaneously.
Personalized Care Plans and Patient Education
Adaptive learning platforms tailor education materials to each patient's literacy level, language preference, and learning style. Interactive tools allow individuals to practice skills like wound care or glucose monitoring in low-stakes environments before performing them independently at home.
This personalized approach to health literacy builds true self-efficacy rather than rote compliance, creating lasting capabilities that prevent readmissions long after formal discharge support ends.
The Role of Community Resources in Preventing Readmissions
Hospital-community partnerships are evolving from referral networks to integrated care ecosystems. Shared data platforms allow social service organizations to coordinate support around high-risk patients, while community health workers serve as cultural bridges between clinical teams and diverse populations.
These collaborative models recognize that health happens everywhere—not just in medical facilities—and that sustainable prevention requires engaging all aspects of patients' lives and environments.