Virtual Reality in Diagnostic Training
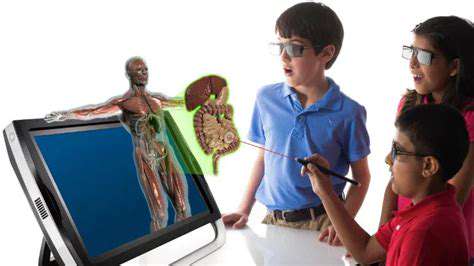
The medical education landscape is undergoing a seismic shift thanks to virtual reality (VR) technology, especially in diagnostic training. Unlike traditional methods, VR creates immersive, risk-free environments where healthcare professionals can repeatedly practice complex procedures. This hands-on approach accelerates skill mastery while eliminating patient safety concerns. Trainees report higher engagement levels and better knowledge retention compared to textbook learning or passive observation.
What sets VR apart is its ability to recreate nuanced clinical scenarios with startling accuracy. From rare disease presentations to difficult patient interactions, these simulations mirror real-world challenges. Instructors can customize variables to create progressively complex cases, allowing learners to methodically build diagnostic competencies. This dynamic training model produces clinicians who are better prepared for the unpredictable nature of medical practice.
Benefits and Applications of VR Diagnostic Simulations
Beyond safety, VR simulations offer unparalleled educational depth. By incorporating actual patient data, high-fidelity imaging, and precise anatomical models, they bridge the gap between theory and practice. Trainees develop not just technical skills but also the clinical reasoning needed for accurate diagnoses. The technology's versatility spans multiple specialties - whether practicing cardiac catheterization or interpreting neurological scans, VR provides realistic procedural training.
The instant feedback feature revolutionizes learning efficiency. As trainees make diagnostic decisions, the system provides real-time assessments, creating a continuous improvement loop. This feature proves equally valuable for seasoned practitioners through continuing medical education (CME) modules. Collaborative VR platforms take learning further by enabling case discussions and team-based diagnosis practice, cultivating essential communication skills.
Perhaps most importantly, VR systems evolve alongside medical advancements. Regular content updates ensure training reflects current best practices and emerging technologies. This adaptability makes VR an enduring asset in medical education's future.
Tailored Training for Specific Medical Conditions

Customized Learning for Healthcare Professionals
Specialized training programs address medicine's increasing complexity by targeting specific competency gaps. This precision approach yields measurable improvements in clinical performance and patient outcomes. Unlike generic courses, these programs adapt content to individual learning paces and specialty requirements, maximizing educational ROI.
The curriculum dynamically incorporates breakthrough research and technological innovations. Such responsiveness ensures practitioners stay ahead in fields where outdated knowledge can have serious consequences. This commitment to continuous learning elevates overall care standards while fostering professional growth cultures within healthcare institutions.
Condition-Specific Training Modules
From robotic surgery techniques to novel diagnostic algorithms, focused modules deliver intensive skill development. These programs often use competency-based progression systems, ensuring mastery before advancement. The tiered structure accommodates varying experience levels - new graduates and veteran clinicians alike find value in the targeted instruction.
Public health crises highlight the modules' importance. When emerging diseases surface or treatment paradigms shift, rapid-response training ensures frontline readiness. Similarly, chronic disease management programs help address growing global health burdens through preventive strategies.
Measuring Training Impact
Effective programs employ multidimensional assessment strategies. Beyond standard testing, they track behavioral changes in clinical settings and patient outcome improvements. This data-driven approach identifies successful components while flagging areas needing refinement. Regular evaluation cycles create a feedback mechanism that keeps training content clinically relevant and educationally effective.
Longitudinal studies demonstrate that institutions prioritizing such assessments see significant care quality improvements. The correlation between rigorous training evaluation and enhanced patient safety makes this component non-negotiable for modern medical education.