The Need for Precision
The field of anesthesia is undergoing a transformative shift toward personalized medicine. While traditional dosing methods rely on generalized guidelines, these often fail to account for individual patient differences, potentially leading to suboptimal outcomes. Tailoring anesthesia to each patient's unique physiology isn't just beneficial - it's becoming essential for modern surgical care. Research shows significant variability in how patients metabolize anesthetic agents, making standardized approaches increasingly obsolete.
Modern anesthesiology recognizes that factors like genetic makeup, body composition, and even emotional state can dramatically affect drug response. Cutting-edge computational models now enable clinicians to predict these variations with unprecedented accuracy, moving beyond the limitations of traditional protocols. This paradigm shift represents a fundamental change in how we approach patient care in the operating room.
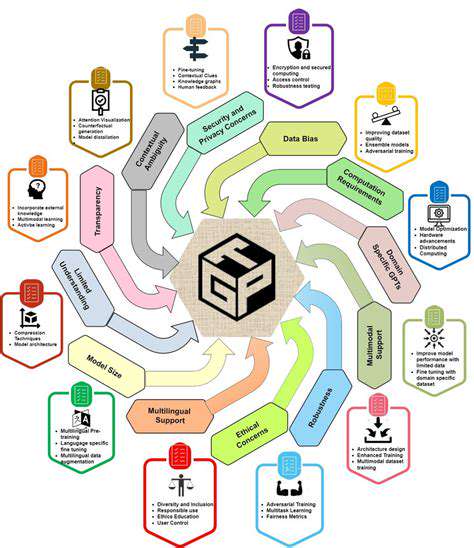
AI's Transformative Impact on Data Analysis
Contemporary anesthesia practice generates enormous datasets, from preoperative assessments to intraoperative monitoring. Advanced analytical tools can process this information in ways that human practitioners simply cannot match. By examining patterns across thousands of cases, these systems identify subtle correlations that inform better clinical decisions.
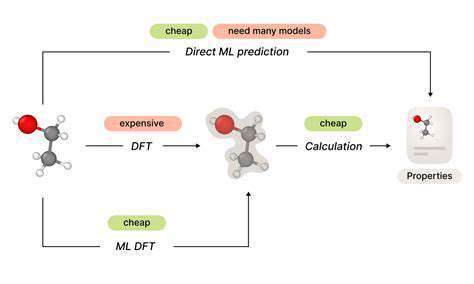
Machine learning applications in anesthesia now routinely incorporate dozens of variables - from basic demographics to complex pharmacogenomic data. This multidimensional analysis creates dosing recommendations that adapt to each patient's specific needs, representing a quantum leap forward from conventional weight-based calculations. The result? Fewer complications and more predictable surgical outcomes.
Enhancing Safety Through Precision Medicine
The clinical benefits of AI-assisted dosing extend far beyond theoretical improvements. Real-world studies demonstrate measurable reductions in postoperative complications when using personalized anesthesia protocols. Particularly notable are decreases in respiratory events and cardiovascular instability - two of the most common anesthesia-related adverse events.
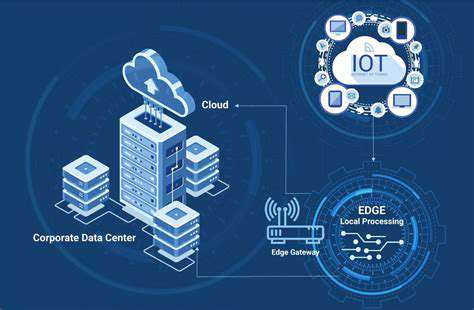
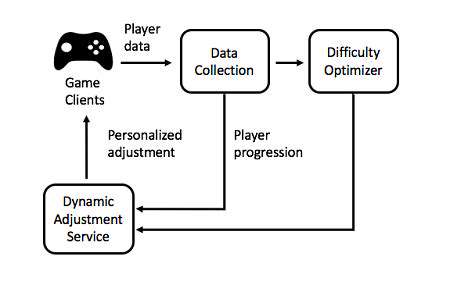
Modern monitoring systems now integrate with AI platforms to provide continuous feedback during procedures. This creates a dynamic dosing environment where anesthetic delivery adjusts in real-time to changing patient conditions. Such responsive systems represent the future of intraoperative care, making anesthesia both safer and more effective.
Predictive Analytics in Anesthetic Management
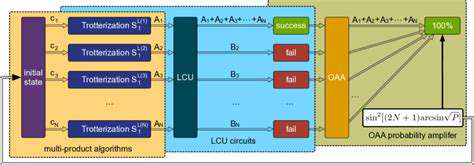
The predictive capabilities of modern AI systems go beyond simple dose calculations. Sophisticated algorithms can now forecast individual responses to specific drug combinations, accounting for complex pharmacokinetic interactions. This predictive power enables clinicians to select not just the right dose, but the optimal drug regimen for each patient - a critical advantage in complex cases.
Optimizing the Patient Experience
Personalized anesthesia delivers tangible benefits that patients can feel. By precisely matching drug delivery to individual metabolism, patients experience smoother inductions, more stable intraoperative conditions, and faster recoveries. This translates to less postoperative nausea, reduced pain, and shorter recovery room stays - outcomes that matter deeply to patients and providers alike.
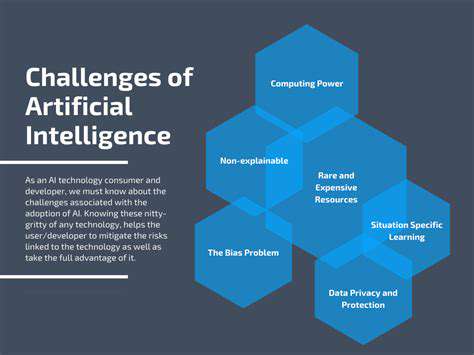
Ethical Implementation of AI in Anesthesia
As with any medical advancement, the integration of AI into anesthesia practice requires thoughtful oversight. Maintaining rigorous validation standards ensures these powerful tools enhance rather than replace clinical judgment. Current research emphasizes the importance of maintaining human oversight while leveraging AI's analytical strengths.
The future promises even greater integration of AI across all phases of anesthetic care. Ongoing studies are exploring how to incorporate real-time biomarkers and advanced imaging data to further refine dosing algorithms. This evolution will continue to push anesthesia toward truly individualized medicine.
Improving Anesthesia Safety and Efficiency
Comprehensive Approaches to Anesthetic Care
Modern anesthesia practice demands a holistic approach to patient safety. The perioperative period represents a complex interplay of physiological systems, requiring careful coordination across multiple care teams. Today's best practices emphasize system-wide strategies that address safety at every phase.
The Critical Role of Preoperative Evaluation
A thorough preoperative assessment forms the foundation of safe anesthesia. Beyond standard history-taking, contemporary evaluations now incorporate detailed risk stratification tools. Identifying potential complications before surgery allows for proactive management rather than reactive crisis control. This shift toward anticipatory medicine has significantly improved outcomes.
Medication reconciliation deserves particular attention, as polypharmacy becomes increasingly common. Detailed pharmacological reviews now routinely include herbal supplements and recreational substances that might interact with anesthetic agents.
Advanced Monitoring: Beyond Basic Vital Signs
Today's operating rooms feature monitoring capabilities unimaginable a generation ago. From advanced EEG monitoring to continuous cardiac output measurement, these technologies provide unprecedented visibility into patient status. This wealth of data enables minute-by-minute adjustments to anesthetic depth and hemodynamic support, preventing complications before they become critical.
Risk Mitigation Strategies
Contemporary anesthesia protocols emphasize preventive approaches to common complications. Tailored strategies for aspiration prevention, temperature management, and hemodynamic stability have become standard practice. These evidence-based interventions collectively reduce adverse events while improving both safety and efficiency.
The Human Element in Patient Comfort
Technological advances complement rather than replace the art of patient-centered care. Effective communication, preoperative education, and attention to emotional needs remain integral to quality anesthesia. Studies confirm that addressing psychological factors improves both subjective experience and objective outcomes.
Postoperative Care: Completing the Continuum
The anesthesia team's responsibility extends well beyond the operating room. Coordinated postoperative care significantly impacts recovery quality and reduces readmission rates. Enhanced recovery after surgery (ERAS) protocols exemplify this comprehensive approach, integrating anesthesia management with surgical and nursing care.
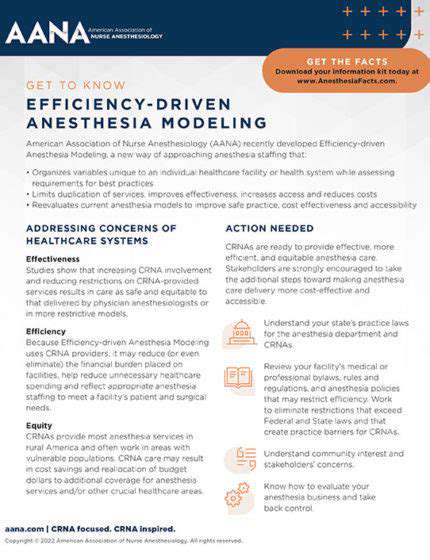
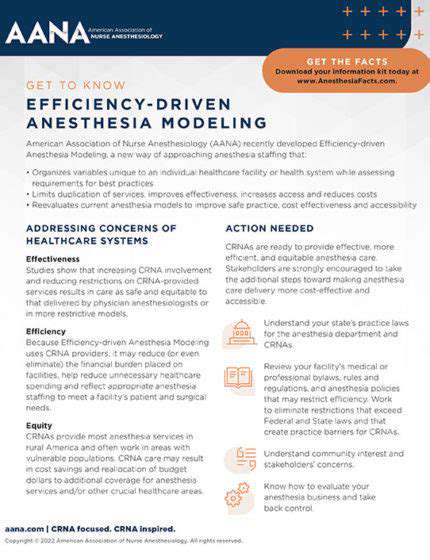
Operational Excellence in Anesthesia
Efficiency improvements in anesthesia practice benefit both patients and healthcare systems. Standardized protocols, optimized workflow designs, and intelligent resource allocation all contribute to better outcomes. When implemented thoughtfully, these operational improvements enhance rather than compromise patient safety, demonstrating that quality and efficiency can be complementary goals.