The Growing Role of AI in Medical Imaging Analysis

AI-Powered Diagnostics
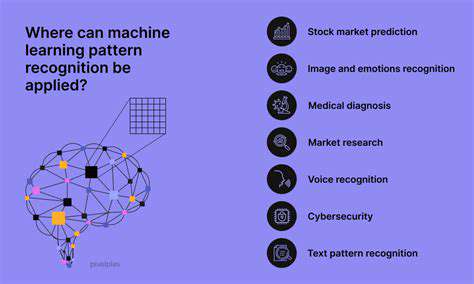
Artificial intelligence (AI) is rapidly transforming the field of medical diagnostics, offering the potential for faster, more accurate, and more accessible diagnoses. AI algorithms can analyze vast amounts of medical data, including images, lab results, and patient history, to identify patterns and anomalies that might be missed by human clinicians. This capability is particularly valuable in areas like radiology, where AI can assist in detecting subtle signs of diseases like cancer or cardiovascular problems.
By automating the analysis of medical images, AI can significantly reduce the workload on radiologists and potentially decrease diagnostic errors. Furthermore, AI can facilitate the early detection of diseases, potentially leading to earlier interventions and improved patient outcomes.
Personalized Treatment Plans
AI's ability to process and analyze complex data is revolutionizing the way treatment plans are developed. By considering individual patient characteristics, medical history, and genetic predispositions, AI can recommend personalized treatment strategies that optimize outcomes and minimize side effects. This approach is particularly beneficial in oncology, where AI can help tailor chemotherapy regimens and radiation therapies to individual patients, maximizing efficacy and minimizing toxicity.
AI algorithms can also predict patient responses to different treatments, allowing physicians to make more informed choices about which therapies are most likely to be effective. This predictive capability can lead to more efficient resource allocation and improved patient care.
Drug Discovery and Development
AI is playing an increasingly important role in the drug discovery and development pipeline. AI algorithms can analyze vast datasets of chemical compounds and biological targets, accelerating the identification of potential drug candidates. This process can significantly shorten the time and cost associated with bringing new medicines to market.
Furthermore, AI can simulate the effects of drugs on different biological systems, helping to identify potential side effects and optimize drug efficacy. This capability is crucial in ensuring the safety and effectiveness of new medications.
Improving Patient Care and Access
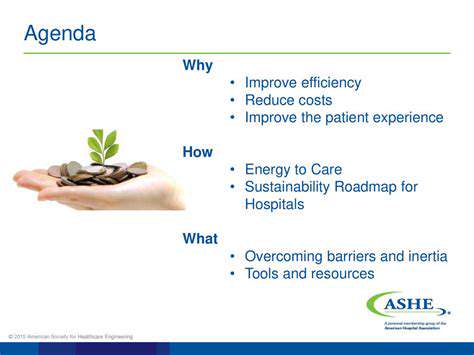
AI is transforming the way healthcare is delivered, making it more accessible and efficient. AI-powered chatbots and virtual assistants can provide patients with 24/7 access to information and support. This increased accessibility can be particularly beneficial for patients in remote areas or those with limited access to traditional healthcare services.
AI can also streamline administrative tasks, such as scheduling appointments and managing patient records, freeing up healthcare professionals to focus on direct patient care. Ultimately, AI has the potential to improve the overall quality of patient care and access to medical resources.
Personalized Cancer Treatment Strategies with AI

Personalized Cancer Treatment Strategies
Personalized cancer treatment strategies are rapidly evolving, moving away from a one-size-fits-all approach towards tailored interventions based on individual patient characteristics. This approach considers a patient's specific tumor type, genetic makeup, and overall health status to develop a treatment plan that is most likely to be effective and minimize side effects. This precision medicine approach is revolutionizing cancer care, leading to improved outcomes and a better quality of life for many patients.
The cornerstone of personalized cancer treatment lies in understanding the unique genetic landscape of a patient's cancer. This involves analyzing the tumor's DNA and RNA to identify specific mutations, gene fusions, and other genetic alterations that drive the cancer's growth and spread. This detailed genetic profile helps clinicians to choose targeted therapies that are more likely to be effective against the specific cancer cells.
Molecular Profiling and Targeted Therapies
Molecular profiling, a key component of personalized cancer treatment, allows clinicians to identify specific genetic alterations within a patient's tumor. This information is then used to select targeted therapies, which are drugs designed to attack specific molecules or pathways involved in cancer development. These targeted therapies often have fewer side effects compared to traditional chemotherapy, as they are designed to specifically target cancer cells, minimizing damage to healthy tissues.
Targeted therapies are revolutionizing cancer treatment by offering more effective and less toxic options. These therapies have shown remarkable success in treating certain types of cancers, particularly those with specific genetic mutations. However, the success of personalized medicine depends on accurate and timely molecular profiling to ensure that the right treatment is selected for the right patient.
Immunotherapy and Immune Checkpoint Inhibitors
Immunotherapy, a rapidly growing field in cancer treatment, harnesses the body's own immune system to fight cancer cells. This approach involves using drugs that enhance the immune response against tumors, either by boosting the activity of immune cells or by blocking proteins that prevent immune cells from attacking cancer cells. This personalized strategy is particularly effective in certain types of cancer.
Immune checkpoint inhibitors are a class of immunotherapy drugs that block these checkpoints, allowing the immune system to recognize and destroy cancer cells more effectively. They have demonstrated remarkable success in treating various cancers, including melanoma, lung cancer, and kidney cancer. However, individual responses to immunotherapy can vary significantly, and further research is needed to optimize their use in personalized cancer treatment.
Integration of Patient Factors and Outcomes
Personalized cancer treatment isn't just about the tumor; it also considers the patient's overall health, lifestyle, and preferences. Factors such as age, other medical conditions, and the patient's willingness to participate in treatment are important considerations in the decision-making process. This holistic approach aims to tailor the treatment plan to each patient's unique needs and circumstances, maximizing the chances of a positive outcome.
Ultimately, the goal of personalized cancer treatment is to improve outcomes and quality of life for cancer patients. By understanding the specific genetic and molecular characteristics of a patient's cancer, clinicians can select the most effective and least toxic treatment options, leading to better outcomes and a more positive experience for patients throughout their journey.
Overcoming Challenges and Ensuring Ethical Considerations
Data Privacy and Security
Protecting patient data is paramount in any medical application, especially when dealing with sensitive information like medical histories and genetic data. AI systems processing such data must adhere to strict privacy regulations, such as HIPAA in the US and GDPR in Europe. This necessitates robust encryption methods, secure data storage protocols, and stringent access controls to prevent unauthorized access and breaches. Implementing these measures is crucial to maintain public trust and ensure the ethical use of patient information in AI-assisted oncology.
Moreover, transparency in data handling is essential. Patients and healthcare providers need clear explanations of how their data is being used by the AI system, and what safeguards are in place to protect it. This includes details on data anonymization techniques and the measures taken to prevent re-identification of individuals from aggregated datasets. Transparency builds trust and fosters confidence in the ethical application of AI in oncology.
Bias Mitigation in AI Models
AI models are trained on data, and if that data reflects existing societal biases, the AI system can perpetuate and even amplify those biases in its predictions and recommendations. In oncology, this could lead to unequal access to treatment or incorrect diagnoses for certain patient demographics. Therefore, meticulous attention must be paid to identifying and mitigating bias in the training data and model architecture. This includes diverse and representative datasets, careful consideration of the features used in model training, and ongoing monitoring to assess and correct for biases as they emerge.
Rigorous testing and validation of AI models on diverse populations are also critical. This process ensures that the model's performance is consistent across different patient groups and minimizes the risk of discriminatory outcomes. Continuous evaluation and adjustment of the AI system are necessary to ensure fairness and equitable access to high-quality care for all patients.
Ensuring Explainability and Interpretability
One of the major challenges in implementing AI in oncology is ensuring that the decision-making process of the AI system is understandable and explainable to both healthcare professionals and patients. Black box AI models, where the internal workings are opaque, can hinder trust and limit the ability to identify and correct errors. Developing AI systems that offer insights into their reasoning and provide clear explanations for their predictions is therefore crucial.
This explainability is essential for building confidence in the AI system's recommendations. For example, when an AI system suggests a particular treatment plan, healthcare providers and patients need to understand the rationale behind the suggestion. This understanding allows for critical evaluation, potential adjustments, and ultimately, better decision-making in patient care.
Validation and Robustness of AI Predictions
The accuracy and reliability of AI-generated predictions in oncology are paramount. AI models must be rigorously validated using diverse and representative datasets to ensure that their performance is consistent and reliable. This validation process should include comparisons with established clinical guidelines, expert opinions, and traditional diagnostic methods. Only through extensive testing and validation can we build confidence in the reliability of AI-assisted diagnoses and treatment plans.
Furthermore, the AI system needs to be robust enough to handle unexpected or novel data points. The ability to adapt and adjust to new information is critical for ensuring the long-term effectiveness of the system in a dynamic clinical environment. Regular updates and retraining of the AI model are essential to maintain its accuracy and reliability in the face of evolving medical knowledge and new patient presentations.
Clinical Integration and Collaboration
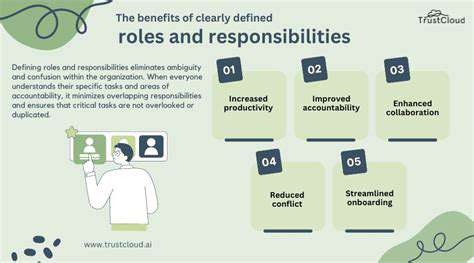
Successfully integrating AI into the clinical workflow requires careful planning and collaboration between AI developers, clinicians, and healthcare administrators. This collaboration is essential to ensure that the AI system is effectively integrated into existing processes and that the benefits are realized in a sustainable and ethical manner. Clear communication channels and established protocols are necessary for seamless integration and efficient utilization of the AI tools.
Ethical Oversight and Regulatory Compliance
Establishing clear ethical guidelines and regulatory frameworks for the development and deployment of AI in oncology is crucial. These frameworks must address issues such as data privacy, bias mitigation, explainability, and accountability. Independent oversight bodies can play a crucial role in monitoring the ethical application of AI and ensuring compliance with relevant regulations. This is essential to maintain public trust and ensure that AI technologies are used responsibly and ethically to improve patient care.
Furthermore, ongoing dialogue and collaboration between stakeholders, including researchers, clinicians, ethicists, and policymakers, are vital for establishing and adapting these guidelines to the evolving landscape of AI technology in medicine.