Personalized Medicine and Drug Response Prediction
Personalized Medicine: Tailoring Treatments to Individuals
Personalized medicine represents a paradigm shift in healthcare, moving away from a one-size-fits-all approach to treatments and towards a more precise and effective strategy. This approach recognizes that individuals respond differently to various drugs and therapies based on their unique genetic makeup, lifestyle, and environmental factors. This tailored approach promises to improve treatment outcomes and reduce adverse effects by selecting the most appropriate therapy for each patient.
By considering individual characteristics, personalized medicine aims to optimize therapeutic interventions and minimize unnecessary or harmful side effects. This approach is particularly crucial in complex diseases like cancer, where genetic variations significantly influence treatment response.
Drug Response Variability: The Need for Individualization
Drug response variability is a significant challenge in traditional medicine. A medication effective for one patient might be ineffective or even harmful for another. This variability stems from genetic differences, environmental factors, and other individual characteristics. Understanding the factors influencing drug response is crucial for developing personalized treatment strategies.
The variability in how people metabolize and respond to drugs necessitates a more nuanced approach to prescribing. Recognizing individual differences allows for adjustments in dosage and drug selection, ultimately improving patient outcomes.
Genetic Factors in Drug Metabolism
Genetic variations play a pivotal role in drug metabolism and response. Certain genes encode enzymes responsible for breaking down drugs in the body. Variations in these genes can affect how quickly or slowly a drug is metabolized, impacting its effectiveness and potential for side effects. Understanding these genetic variations is crucial for tailoring drug dosages and selecting appropriate medications.
Genetic testing can identify these variations, providing valuable insights into an individual's drug metabolism capabilities. This information can be used to optimize drug therapy, minimizing adverse reactions and maximizing treatment efficacy.
Pharmacogenomics: The Science Behind Personalized Medicine
Pharmacogenomics is the study of how genes affect a person's response to drugs. It combines pharmacology (the study of drugs) with genomics (the study of genes) to identify genetic variations that influence drug metabolism, efficacy, and toxicity. This field is rapidly advancing, leading to increasingly sophisticated tools for predicting individual drug responses.
Pharmacogenomic research is focused on identifying specific genetic markers that correlate with drug response. This knowledge will revolutionize treatment strategies, enabling healthcare professionals to select the most effective medication for each individual and avoid adverse drug reactions.
Personalized Drug Discovery and Development
Personalized medicine is not just about tailoring existing treatments; it's also revolutionizing drug discovery and development. Researchers are now incorporating genetic information into the process of identifying and developing new drugs. This approach aims to create drugs that are more effective and have fewer side effects by targeting specific genetic pathways.
By understanding the genetic basis of disease and drug response, researchers can design more targeted therapies. This personalized approach to drug development promises to shorten the drug discovery process and significantly reduce the risk of failures in clinical trials.
Clinical Applications of Personalized Medicine
The clinical applications of personalized medicine are already transforming various fields of healthcare. In oncology, personalized therapies are being used to target specific cancer-causing genes and mutations, leading to more effective and less toxic treatments. This approach is also being applied to other chronic conditions, such as cardiovascular disease and psychiatric disorders, offering tailored treatment strategies.
Ethical Considerations and Future Directions
As personalized medicine continues to advance, ethical considerations become increasingly important. Issues such as data privacy, access to testing, and potential biases in genetic information need careful consideration. The future of personalized medicine hinges on responsible development and implementation of these technologies and protocols, ensuring equitable access and minimizing potential harm.
Future research should focus on addressing these challenges and ensuring that personalized medicine benefits all individuals, regardless of their socioeconomic status or background. This includes developing cost-effective genetic testing and training healthcare professionals in the use of personalized medicine approaches.
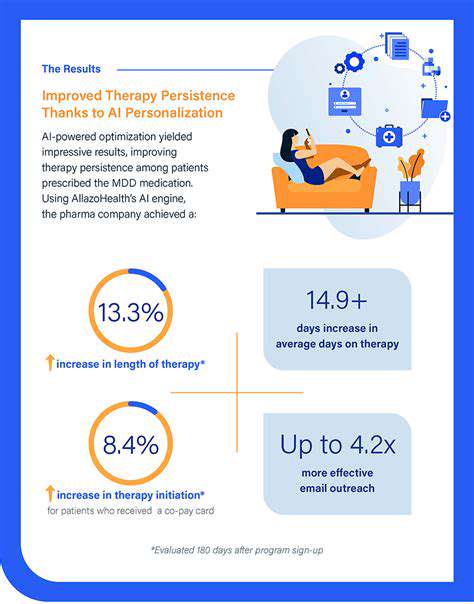
Enhancing Efficiency and Reducing Costs
Accelerated Drug Target Identification
Artificial intelligence (AI) is revolutionizing drug discovery by drastically accelerating the identification of potential drug targets. Sophisticated algorithms can sift through vast datasets of biological information, including genomic sequences, protein structures, and clinical trial data, to identify molecules and pathways that are crucial for disease progression. This accelerated process, compared to traditional methods, significantly shortens the time it takes to pinpoint promising targets, potentially leading to faster development of new treatments.
By analyzing complex interactions within biological systems, AI can identify intricate relationships and pathways that might be missed by human researchers. This ability to uncover hidden connections holds immense promise for discovering novel therapeutic targets, opening doors to new avenues for treating diseases previously considered intractable.
Optimized Drug Design and Development
AI plays a critical role in optimizing drug design, enabling the creation of more effective and safer medications. Machine learning algorithms can analyze vast datasets of existing drug structures and their properties to predict the efficacy and toxicity of potential new drug candidates. This predictive capability allows researchers to focus on compounds with the highest probability of success, reducing the time and resources spent on less promising candidates.
Enhanced Screening and Selection Processes
Traditional drug screening methods often rely on laborious and time-consuming experiments. AI-powered high-throughput screening platforms can significantly enhance these processes, enabling the rapid evaluation of thousands or even millions of compounds in a fraction of the time. This accelerated screening enables researchers to identify potential lead compounds with desired properties more efficiently.
Further, AI algorithms can analyze the results of these screens, identifying patterns and trends that would be difficult to discern manually, leading to more informed decisions regarding compound selection and further development.
Predictive Modeling for Clinical Trials
AI-powered predictive models can be used to forecast the potential success of clinical trials, enabling researchers to allocate resources more effectively. By analyzing historical data and incorporating real-time information about patient populations and treatment responses, these models can predict the likelihood of a drug achieving its desired outcomes, potentially leading to more successful and efficient clinical trial designs.
Reduced Costs and Time-to-Market
By accelerating the identification of drug targets, optimizing drug design, and enhancing screening processes, AI significantly reduces the overall time and cost associated with drug discovery. This efficiency translates to faster time-to-market for new drugs, getting life-saving treatments into the hands of patients sooner and maximizing the return on investment for pharmaceutical companies.
Improved Safety and Efficacy Predictions
AI's ability to analyze vast datasets allows for more accurate predictions of drug safety and efficacy. By identifying potential side effects and adverse reactions early in the development process, AI minimizes the risk of costly and time-consuming setbacks later on. This proactive approach enhances the safety profile of the final drug candidate, ultimately leading to a more reliable and beneficial treatment.