Ethical Considerations and the Future of AI in Substance Abuse Treatment
Transparency and Explainability
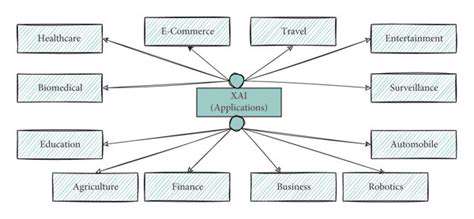
The growing role of artificial intelligence in addiction therapy demands absolute clarity in how these systems operate. People undergoing treatment deserve to know exactly how AI-generated suggestions are formulated, including the specific data points analyzed, algorithmic processes involved, and rationale for proposed interventions. Without this visibility, skepticism may grow and patients might disengage from potentially life-saving technologies. Honest discussions about AI's current limitations, combined with professional supervision, form the foundation for establishing credibility and ensuring proper implementation.
Explainable artificial intelligence (XAI) approaches play a pivotal role in creating trustworthy systems. When treatment providers can examine the reasoning behind AI-generated conclusions, they gain valuable perspective on the critical factors influencing therapeutic suggestions. This transparency enables more productive discussions between clinicians and patients, leading to treatment plans that better address individual circumstances.
Data Privacy and Security
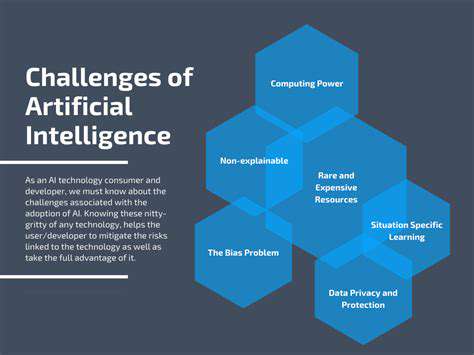
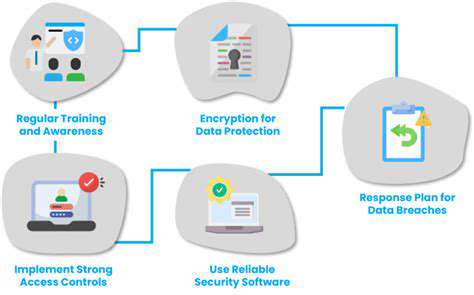
Safeguarding personal health information represents a fundamental requirement in all medical contexts, but takes on heightened importance when dealing with addiction treatment records. Details about a person's recovery journey contain exceptionally sensitive material requiring the strictest protection protocols. Comprehensive cybersecurity defenses must prevent any unauthorized data access, with rigorous compliance to privacy laws such as HIPAA being non-negotiable.
Effective protection strategies incorporate multiple layers of security including advanced encryption methods, secure data storage solutions, and carefully managed access permissions. Additionally, well-defined guidelines governing information management should be developed and clearly explained to everyone involved in patient care.
Bias Mitigation and Fairness
Since machine learning algorithms learn from historical data, they risk reinforcing societal prejudices present in their training material. This could result in unequal treatment recommendations that disadvantage specific population groups, potentially worsening existing healthcare disparities among those seeking help for substance use disorders.
Treatment programs must carefully examine the potential for prejudicial elements within datasets used to develop AI models. Continuous evaluation of algorithmic decision-making for signs of partiality, along with corrective measures when biases are detected, remains essential for guaranteeing fair treatment opportunities across all patient demographics.
Accountability and Responsibility
Assigning liability when AI systems deliver incorrect or potentially harmful advice presents significant challenges. Defining precise responsibility boundaries between healthcare professionals, software engineers, and healthcare organizations ensures proper supervision and timely resolution of issues. When technology contributes to adverse outcomes, clearly identifying responsible parties becomes critical for patient protection and system enhancement.
Effective safeguards include built-in error detection within AI platforms, combined with human review procedures and intervention protocols. Routine performance evaluations help detect emerging concerns and guide necessary adjustments, supporting ongoing refinement of these tools. Such comprehensive oversight guarantees ethical operation while maximizing the therapeutic value of AI-assisted treatment approaches.
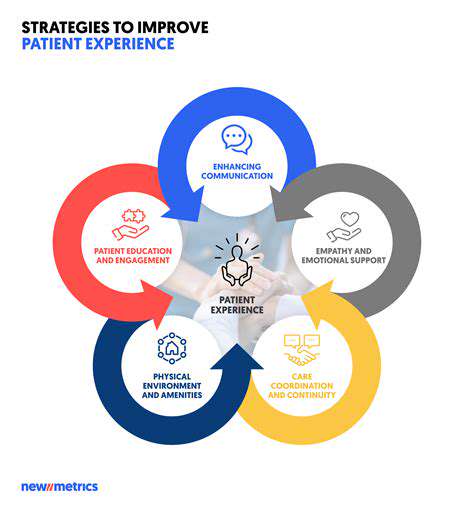
The Role of Human Clinicians in the Era of AI
Despite technological advancements, the human element remains indispensable in addiction treatment. While AI can streamline administrative tasks, offer analytical insights, and support personalized care strategies, the nuanced understanding, emotional intelligence, and therapeutic connection provided by trained professionals cannot be replicated by machines. Healthcare providers serve as essential interpreters of algorithmic output, ethical safeguards for technology implementation, and primary sources of human compassion throughout the recovery process.
The most effective treatment models will likely combine the analytical strengths of artificial intelligence with the irreplaceable human qualities of experienced clinicians. This synergistic approach keeps patient welfare at the forefront while harnessing the complementary capabilities of both human expertise and machine intelligence. Preparing addiction specialists to properly utilize and contextualize AI-generated information represents a critical step toward successful integration of these technologies in clinical practice.