Pre-operative Planning and Risk Assessment
Pre-operative Assessment
Conducting an exhaustive pre-operative evaluation stands as a cornerstone in assessing a patient's readiness for surgery and pinpointing possible hazards. This process requires an in-depth examination of the individual's complete medical background, covering prior health issues, allergic reactions, current medications, and any past surgical interventions. A meticulous analysis of the patient's present physical state proves indispensable, incorporating vital measurements, laboratory findings, and diagnostic imaging. Such scrutiny enables the detection of any covert conditions that could potentially complicate the surgical intervention or heighten the probability of adverse events.
Surgical Risk Factors
Multiple elements can impact the likelihood of surgical complications. These encompass age, underlying health conditions such as heart disease, diabetes, or respiratory disorders, along with the intricacy of the proposed operation. Thoughtful evaluation of these variables plays a pivotal role in establishing the necessary pre-operative care and support level. Recognizing these risk components empowers medical practitioners to formulate well-informed choices concerning patient readiness and possible preventative measures.
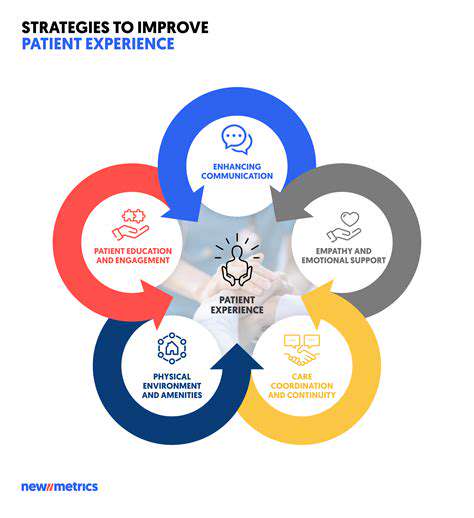
Patient Preparation and Education
Comprehensive patient readiness forms the bedrock of favorable surgical results. This involves delivering unambiguous information regarding the procedure, potential hazards and advantages, and anticipated recovery milestones. Guaranteeing that patients grasp the significance of adhering to pre-operative directives, including dietary restrictions and medication modifications, stands as a critical priority. This preparatory phase also incorporates addressing patient apprehensions and queries, promoting a cooperative healthcare approach.
Anesthesia Considerations
Anesthesia constitutes a vital aspect of surgical interventions, necessitating thorough evaluation of the patient's medical background and physical status. Choosing the optimal anesthetic method and vigilantly tracking patient responses during the procedure remains fundamental for risk mitigation and safety assurance. Parameters such as patient age, body mass, and any pre-existing respiratory or cardiovascular conditions demand careful scrutiny prior to anesthesia administration.
Intraoperative Management
Effective intraoperative management requires unwavering attention to detail throughout the surgical process. This incorporates strict observance of sterile protocols, continuous vital sign monitoring, and immediate response to any emerging complications. Sustaining transparent communication among surgical staff and anesthesia providers proves essential for efficient intraoperative oversight. Such coordination enables prompt reaction to unforeseen developments and optimizes procedural outcomes.
Post-operative Planning
Post-surgical strategizing holds equivalent importance to pre-operative preparations. This entails anticipating possible complications like hemorrhage, infection, or discomfort and formulating appropriate management approaches. A meticulously structured post-operative regimen, featuring pain control methods, wound care guidelines, and scheduled follow-ups, remains vital for patient rehabilitation and complication prevention. This guarantees patients obtain suitable assistance post-surgery, easing their return to normal activities.
Intraoperative Guidance and Assistance

Intraoperative Navigation Systems
Contemporary intraoperative navigation systems represent cutting-edge technology offering real-time, pinpoint accuracy during surgical operations. These platforms utilize sophisticated imaging modalities, frequently integrating CT, MRI, or fluoroscopic data to generate three-dimensional anatomical reconstructions. Such technology enables surgeons to examine the operative field with unprecedented clarity, improving their comprehension of adjacent structures and promoting more exact surgical strategizing. This level of precision proves indispensable for reducing tissue damage and optimizing success rates.
Minimally Invasive Surgery
Intraoperative guidance technology demonstrates particular value in minimally invasive procedures. These approaches typically involve reduced incision sizes, resulting in decreased patient trauma and accelerated recuperation periods. Clear visualization and exact instrument positioning become critical factors in complication prevention. The capability to virtually inspect deep anatomical structures and manipulate instruments with accuracy substantially enhances these technically demanding operations.
Surgical Planning and Simulation
Pre-surgical preparation assumes a crucial role in successful operative outcomes. Modern guidance systems frequently permit the generation of virtual surgical rehearsals using patient-specific anatomical information. This functionality enables surgeons to practice procedures digitally, recognizing potential challenges and refining their technique. Such preparatory simulations can dramatically shorten the learning curve during actual operations, permitting more assured and proficient surgical performance.
Real-time Feedback and Adjustments
Among the most valuable features of intraoperative guidance technology is its capacity for instantaneous feedback. Surgeons can continuously monitor instrument positioning relative to critical anatomical landmarks. This ongoing input facilitates dynamic modifications during the procedure, ensuring adherence to the surgical blueprint while accommodating necessary adaptations. This flexibility proves fundamental for achieving superior surgical results.
Enhanced Accuracy and Precision
Intraoperative guidance systems substantially improve surgical accuracy and precision. By delivering detailed three-dimensional visualization of the operative site, surgeons can target specific anatomical structures with remarkable exactitude. This precision becomes particularly important for avoiding damage to delicate tissues, organs, or vascular structures, consequently improving patient outcomes through reduced complication rates.
Improved Visualization and Understanding
The advanced visualization capabilities of modern guidance systems afford surgeons an unparalleled comprehension of the operative field. They can examine complex anatomical relationships in ways impossible with conventional techniques. This enhanced understanding markedly decreases error potential and increases procedural predictability. This comprehensive perspective, with its inherent accuracy, serves as a critical tool for enhancing patient safety and minimizing surgical complications.
Improved Post-operative Care and Monitoring
Pre-operative AI Assessment
Advanced computational algorithms can process patient information, incorporating medical background, diagnostic imaging, and genetic profiles to predict potential complications and customize surgical approaches. This forward-looking methodology enables surgeons to foresee risks and create individualized treatment strategies, potentially decreasing the necessity for extensive consultations while improving results.
Early identification of high-risk individuals enables more educated decisions regarding surgical timing and technique selection. This preventive dimension can substantially reduce the probability of unexpected complications throughout the surgical continuum.
Real-time Intraoperative Monitoring
Intelligent monitoring systems can track physiological parameters, operative site conditions, and instrument utilization throughout surgical procedures. This constant data stream permits immediate procedural adjustments, potentially reducing complications and enhancing surgical accuracy. For instance, the technology can identify subtle cardiovascular changes, prompting necessary interventions to maintain optimal patient stability.
Post-operative Complications Prediction
Predictive analytics can examine diverse post-surgical metrics, including patient characteristics, procedural details, and recovery responses to forecast complication probabilities. This anticipatory strategy allows medical teams to implement preventive protocols and intensify monitoring for vulnerable patients. Early complication recognition enables swift intervention, potentially averting serious adverse outcomes.
Personalized Post-operative Care Plans
Advanced algorithms can produce customized recovery plans addressing individual patient requirements. These plans might incorporate pain control recommendations, medication regimens, nutritional guidelines, and rehabilitation protocols. This tailored methodology ensures patients obtain optimally suited care, promoting faster recuperation. This individualized approach also reduces dependence on empirical treatment methods, maximizing post-operative care efficiency.
Enhanced Patient Monitoring and Communication
Intelligent monitoring systems can provide continuous oversight of patient vital signs during recovery. This real-time surveillance facilitates early complication detection and prompt treatment. Additionally, the technology can improve inter-provider communication, enabling more coordinated and effective responses to emerging issues. This integrated communication framework ensures all relevant personnel access critical information, supporting proactive patient management.
Remote Patient Monitoring and Follow-up
Digital health technologies enable distant patient surveillance, permitting continuous data collection from residential settings. This approach enhances patient convenience while minimizing hospital visits. Automated systems can notify healthcare providers about unexpected recovery deviations, facilitating timely interventions. This remote oversight significantly contributes to improved outcomes by enabling convenient yet thorough follow-up care.
Data Analysis for Continuous Improvement
Computational systems aggregate and analyze extensive datasets encompassing surgical procedures, patient outcomes, and recovery protocols. This comprehensive data examination reveals patterns that can optimize surgical methods, refine care standards, and elevate overall patient safety. This evidence-based approach empowers healthcare professionals to continuously enhance their practices through data-driven insights.