Improving Diagnostic Accuracy and Consistency
Improving Diagnostic Efficiency
Accurate and timely diagnosis is crucial in healthcare, impacting patient outcomes and resource allocation. Improving diagnostic efficiency involves streamlining processes, optimizing workflow, and leveraging technology to reduce turnaround times. This can significantly reduce the time patients spend waiting for results, allowing for quicker interventions and better management of their health conditions. Efficient diagnostic procedures can also free up valuable resources for healthcare professionals, enabling them to focus on other crucial aspects of patient care.
One key aspect of improving diagnostic efficiency is the implementation of advanced diagnostic tools and technologies. These tools can often provide faster and more precise results compared to traditional methods, leading to quicker and more effective treatment plans. For example, the integration of AI-powered diagnostic systems can analyze medical images and identify potential anomalies with remarkable speed and accuracy. This automation can significantly reduce the workload on human specialists, allowing them to focus on more complex cases and provide more personalized care.
Enhancing Diagnostic Sensitivity and Specificity
Diagnostic tests should ideally exhibit high sensitivity and specificity. High sensitivity means the test accurately identifies individuals who have the condition, minimizing false negatives. High specificity ensures that the test accurately identifies individuals who do not have the condition, minimizing false positives. These characteristics are crucial for reliable diagnosis and the avoidance of unnecessary interventions or treatments.
Improving the sensitivity and specificity of diagnostic tools can involve various strategies, such as refining existing test methodologies or developing entirely new diagnostic approaches. These efforts can lead to more accurate diagnoses, enabling healthcare providers to make informed decisions regarding patient care and treatment plans. Minimizing false positives and false negatives is essential for avoiding inappropriate interventions, saving resources, and improving patient outcomes.
Utilizing Data Analytics for Improved Diagnostics
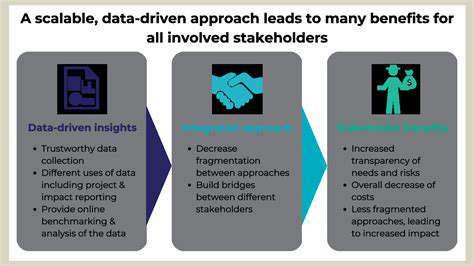
Data analytics plays a pivotal role in enhancing diagnostic accuracy and efficiency. By analyzing large datasets of patient information, including medical history, symptoms, and test results, healthcare professionals can identify patterns and trends that might not be apparent through traditional methods. This can lead to earlier detection of diseases and more precise risk assessments.
Data analytics can be employed to develop predictive models that aid in identifying individuals at high risk of developing certain conditions. These models can assist in targeted screenings and preventative measures. Utilizing data analytics in diagnostic procedures allows for a more proactive and personalized approach to patient care. Predictive models, based on large datasets, can significantly improve the accuracy of diagnoses and aid in the prevention of diseases.
Optimizing Diagnostic Workflow
Streamlining diagnostic workflows is a critical aspect of improving overall diagnostic accuracy. Effective workflows involve optimizing the entire process, from initial patient contact to the final report delivery. This includes establishing clear protocols for sample collection, processing, and analysis, as well as clear communication channels between different departments and healthcare professionals.
Properly trained personnel and well-maintained equipment are essential components of any efficient diagnostic workflow. Implementing and maintaining quality control measures at each stage of the workflow ensures consistency and reliability of results. By optimizing these procedures, healthcare facilities can significantly reduce errors and ensure that diagnostic tests are performed accurately and efficiently.
Challenges and Future Directions
Improving Accuracy and Reliability
A key challenge in applying AI to pathology is ensuring the accuracy and reliability of the analysis. Current AI models, while showing promise, may still struggle with complex or unusual tissue patterns. Further development is needed to enhance their ability to differentiate between benign and malignant cells, especially in cases where the distinction is subtle or ambiguous. This requires larger, more diverse datasets of annotated images to train the models and ensure robustness across various tissue types and disease presentations. Robust validation procedures are also crucial to establish confidence in the AI's diagnostic ability and mitigate the risk of false positives or negatives, which could lead to misdiagnosis and inappropriate treatment.
One area of focus is developing methods for evaluating the uncertainty associated with AI predictions. Knowing the confidence level of an AI's diagnosis is critical for clinical decision-making. This involves incorporating uncertainty quantification techniques into the model training and inference processes. This allows clinicians to weigh the AI's prediction alongside their own expertise and clinical judgment, leading to more informed and comprehensive patient care. Furthermore, establishing clear protocols for interpreting and reviewing AI-generated reports is essential to ensure effective integration into existing workflows and to prevent reliance on the AI alone without proper human oversight.
Addressing Ethical and Regulatory Concerns
The integration of AI into pathology raises important ethical and regulatory considerations. Ensuring data privacy and security of patient information is paramount. Strict adherence to ethical guidelines and regulations, such as HIPAA in the US, is critical to protect patient confidentiality and maintain trust in the system. Furthermore, concerns about bias in AI algorithms trained on existing datasets need to be addressed. Such biases could perpetuate existing inequalities in healthcare access and outcomes. Careful evaluation and mitigation of potential biases are essential to ensure fairness and equitable application of AI in pathology.
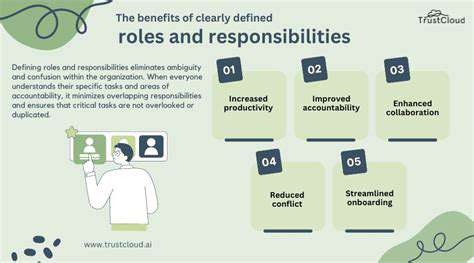
The development of clear guidelines and regulatory frameworks for the use of AI in pathology is another crucial aspect. These guidelines should address the roles and responsibilities of both AI developers and clinicians. This includes defining the scope of AI's application, establishing protocols for validation and verification, and outlining the process for handling discrepancies between AI predictions and human interpretations. These regulatory frameworks will help build confidence and acceptance of AI-driven diagnostic tools within the healthcare community and ensure responsible innovation.
Enhancing Accessibility and Cost-Effectiveness
Making AI-powered pathology tools accessible and cost-effective is crucial for broader adoption. The high initial investment costs associated with developing and implementing these technologies can limit their availability in resource-constrained settings. Finding innovative approaches to reduce the cost of hardware, software, and maintenance is vital. This includes exploring cloud-based solutions and open-source software platforms to enhance affordability and accessibility. Furthermore, strategies for training pathologists and other healthcare professionals on the use and interpretation of AI-generated reports should be developed. This will ensure smooth integration into existing workflows and foster effective collaboration between AI and human expertise.
Developing user-friendly interfaces and intuitive software platforms is essential to ensure accessibility for pathologists of all levels of experience. Simplifying the integration of AI tools into existing pathology workflows will streamline the process and enhance efficiency. This will lead to improved turnaround times for diagnoses and ultimately better patient outcomes. Additionally, exploring the potential for remote access to AI-powered pathology services could improve access to specialized diagnostic capabilities in geographically underserved areas.